Fellow Humans
“Good evening my fellow humans,” Dr. Leslie Farrington projected as she began her talk at the front of a large auditorium in the Sciences Center at Auburn University. She was speaking on behalf of the Pulse Center for Patient Safety Education & Advocacy and the A.S.K. for Your Life campaign. “’Of all the forms of inequality, injustice in healthcare is the most shocking and inhumane.’ Dr. Martin Luther King, Jr. said that.” This quote functioned as an effective primer for the topic of her discussion: Racial disparities and inequities in the healthcare system.
She started with a brief discussion of her background and personal history, explaining that she dedicates the work in her second career to her parents, a White woman and Black man who made a profound impact on her growing up. She then moved to explain biases within the healthcare and the deadly consequences that go with them. To name just a few, speaking on African Americans in comparison to their White counterparts, maternal mortality is four times greater; they die 40% more often from breast cancer, though both groups have the same number of mammograms performed; they are prescribed 50% less pain medication for long bone fractures; and there are 260 premature and preventable deaths of African Americans every day, which reaches nearly 100,000 every year. These biases, whether implicit or explicit, clearly have immense ramifications.
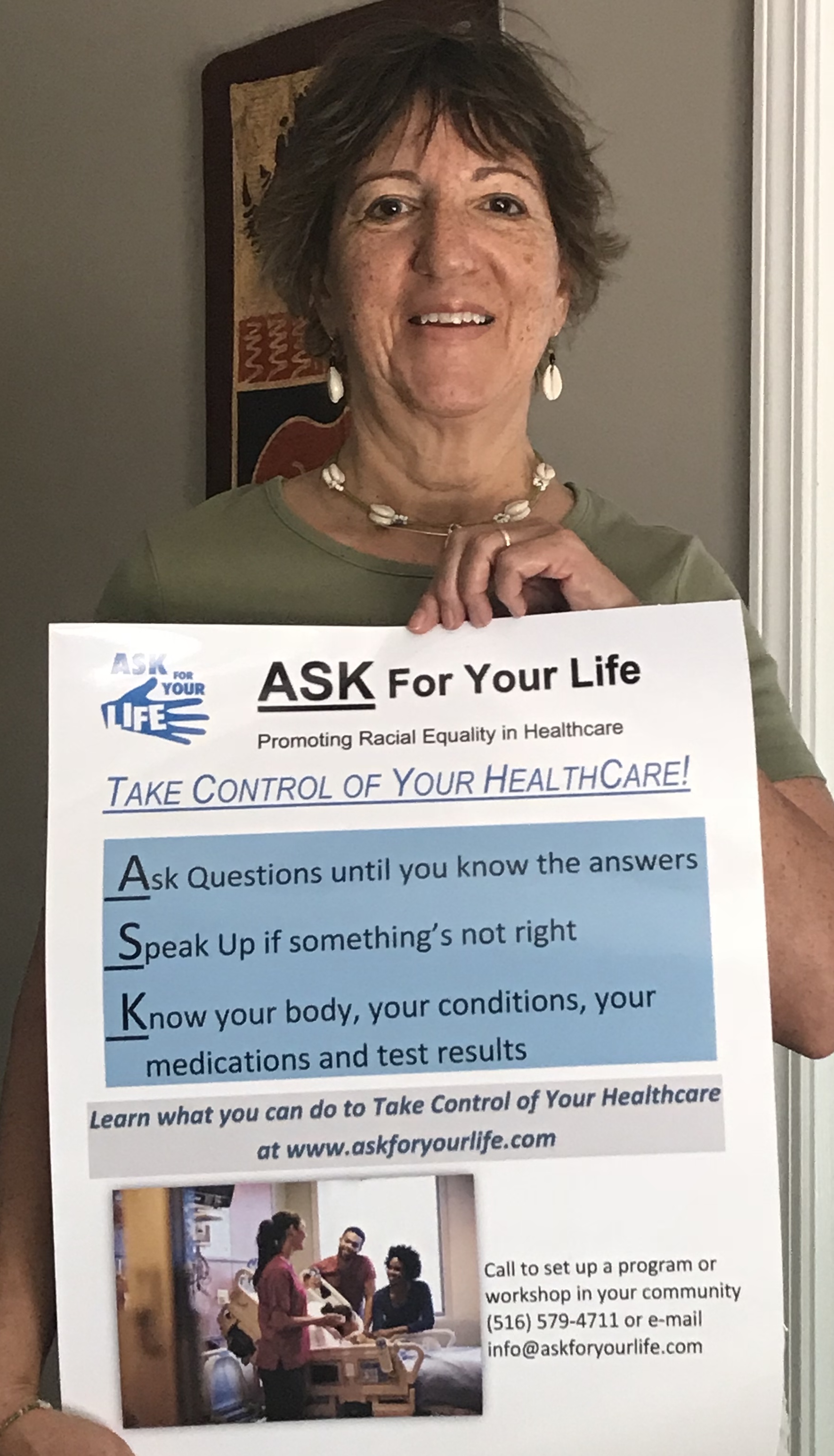
Dr. Farrington with A.S.K. For Your Life
After her talk, Dr. Farrington and I spoke briefly, but it wasn’t until the following afternoon when we sat down for our full interview. Outside, it felt like what I consider to be a typical winter’s day of the American South; cold, windy and gray, which was in stark contrast to the warm, yellow glow of the lobby of the Hotel at Auburn University. Inside, I sat down within a group of large chairs, situated near the draped windows which gave a view of the Hotel’s entrance. Dr. Farrington soon met me with her roller bag in tow, occupying a chair to my left with its back to the windows. As she did so, we discussed the pleasant music floating in the background and the high-quality gymnasium facilities before I asked her about where she grew up.
A Complicated World
“I grew up in Jamaica, New York,” she replied, “which is a part of Queens that is a predominantly Black area.” However, when her mother first moved there, it was inhabited by mostly White people. Over the course of the following few years, though, the demographic changed. She attributed this change to White Flight, which is the phenomenon where a few Black people move in to a neighborhood and all the White people leave. No matter the demographic, she never really felt comfortable socially. “I was the only Black person who looked White,” she told me, which led to her experiencing a profound feeling of social isolation at school and in her neighborhood. People would even go so far as to tell her that she wasn’t Black. “I was quite aware of being different,” she remarked about her childhood. As such, she spent much time home alone reading, which she believes helped her graduate from high school a year early.
Dr. Farrington's Parents
Following her high school graduation, she headed South from Jamaica, New York for Baltimore, Maryland and attended Johns Hopkins University. “There was this small, very close-knit group of Black students, and I was recruited as a Black student,” she informed me. Up to this point in time, which was early in the 1970’s, Johns Hopkins only admitted a handful of Black students each year. Despite their small numbers, the community of Black undergraduate and graduate students embraced one another and, having been accepted as a part of this group, Dr. Farrington experienced what she called her social “coming out.” One of the students referred to her as “high yellow,” a term she had not been familiar with prior, meaning a Black person who has light skin and partial White ancestry. This term doesn’t have particularly warm connotations, but she told me that student was still her friend and it was just how he referred to her. On the other end of the spectrum, the predominantly light-skinned students also tended to voice a negative disposition toward darker-skinned individuals, creating a culture of colorism on the campus. “It’s a complicated world, isn’t it,” she stated matter-of-factly. I agreed.
Dr. Farrington took an interesting route in her undergraduate career at Johns Hopkins. After having completed the coursework for her bachelor’s degree in three years, she took a semester off and then took some pre-med courses. “It was during the course of taking the pre-med courses that I decided I wasn’t going to medical school, because it was too hard,” I laughed empathetically. She graduated, and already having one daughter at the time, she decided to have another baby and see where life took her as a housewife. “That lasted about a year,” she said, and I laughed again, “I can’t just be a housewife.” Bouncing around various schools in the Northeast and East Coast areas over the course of four years, she patched together a pre-med curriculum by taking classes at institutions such as the University of the District of Columbia and Northeastern University. These classes were difficult, and she was sometimes unsure if she could handle some of the science classes involved, but she eventually found if she put her mind to it, she could do as well in these classes as she had done in other classes. After those four years, she felt prepared to apply to medical school, but then a third pregnancy postponed that step for another year.
However, once she did send out her applications, she received three acceptance letters from local universities. Two of these schools had $20,000 tuitions and the third had a much more reasonable tuition of $3,000. That third school was Howard University. “I was happy to go to Howard,” she told me, “it soothed the discomfort of color.” Both of her sisters had also attended Howard University and she had a good experience earning her medical degree there.
A Very Rewarding Way to Practice
After having earned her degree, the newly titled Dr. Farrington wanted to head back to her community in New York, so she applied to residencies back in her home state. Fortunately, the Long Island Jewish Medical Center offered her a position where she split time between two hospitals. Interestingly, one was located right where she grew up in Jamaica! Ever since she had her first child, she knew she wanted to be involved in helping other women deliver children of their own. However, she did originally want to be a midwife, but her husband at the time suggested that it would be easier to get a high-salary job as a physician. “That was one good thing about that marriage,” she quipped, and over my laughter quickly added that her children were too, of course. She spent 20 years at the Long Island Jewish Medical Center practicing obstetrics before moving to a less stressful position practicing office gynecology out of her home, which she practiced for eight years. Speaking about the change in practice, she said, “it was wonderful.” She had the opportunity to spend more time with her patients, which led to the patients themselves being happier; she felt less stressed from the lower volume of patients and stakes of the job at hand; her home office had a great view over the water; the lower income and time commitment helped her to segue into retirement; altogether, she called it a “very rewarding way to practice.”
Then, as she said in her talk the day prior, 2014 happened. “Okay so, I’m volunteering, I joined a church in my community… and I came upon this program,” she told me. At the time, the program was called Pulse of New York, but it eventually came to be known as Pulse Center for Patient Safety, Education and Advocacy. She informed me that when she was a practicing physician, she didn’t truly realize that doctors made mistakes. “It just didn’t register,” she said, “but my eyes and heart started to open up to the issue.” Ilene Corina, who is the president, founder and only full-time employee of Pulse, helped to get Dr. Farrington more and more involved. On behalf of Pulse, Dr. Farrington worked with the National Coalition to Address Maternal Mortality, which is now called the Council on Patient Safety and Women’s Healthcare, as the voice of the patient in the OB-GYN/patient relationship. This council, which was created to address all the ways OB-GYN hasn’t kept up the standards they should to keep women safe and healthy, meant many meetings and innumerable phone calls for Dr. Farrington and marked the starting point for her second career as a healthcare activist.

Dr. Farrington volunteering at Pulse
After learning about her journey to get where she is today, we talked about specific health disparities in the United States. “There are a multitude of inequalities that make up the difference in life expectancy between Blacks and Whites,” she told me. We talked about unconscious racial biases held by healthcare providers and the statistics that showed Black women dying more often than other demographics, even when statistically controlling for socioeconomic status, education level and comorbidity of multiple diseases. In other words, there is scientific evidence that racism within the healthcare system could lead to preventable deaths. “It’s all echoing back to things my father used to say,” she said. “Some Black people are so aware, they’re keenly aware that this goes back generations. They know what’s going on. It doesn’t surprise them that racism is killing us.” As racism is a multifaceted beast inhabiting a pervasive swath of the American experience, there is no single answer to how healthcare providers can address the disproportionate preventable death rate of Black people. However, Dr. Farrington and I did discuss a few possible solutions.
“When I became a physician, everyone was like, ‘ooh, you’re a doctor,’ treating me like I was a princess or something!” she told me. It turns out that putting physicians up on a pedestal, seeing them as all-knowing and perfect, only leads to the growing gulf between healthcare providers and their patients. “If doctors aren’t put on a pedestal and partnered with patients better,” she explained, “they could work better with those patients.” It seems simple but changing any sort of culture takes a lot of both time and effort. In a slightly different vein, we also discussed how health literacy contributes to health discrepancies, though Dr. Farrington dislikes the term literacy. “I don’t know what to call it,” she admits, “[but] it’s not only on patients to find out what they need to know.” She believes that doctors need to be more willing to assist their patients in making decisions that pertain to their health and used the term ‘teamwork’ to more accurately describe how the physician/patient relationship should look.
The Want to Inspire
Continuing to look to the future, I asked Dr. Farrington what she would say to someone who is looking to join the health field. “Well,” she began, “figure out if you want to make money or really help people. Find what you’re passionate about. Biology? Human physiology? That’s what grabbed me… If I’m interested in learning how the body works, then I’m interested in learning chemistry and biology.” Essentially, her passion in human physiology necessitated her learning about the other sciences to which she had an initial aversion. Moreover, she suggested people interested in the health field should volunteer. “See if you really have an inclination to help people. [You have to] have compassion as a basic place where you come from, because if not you probably won’t want to pursue the medical field.” She also told me that ideally, there would be less risk of being sued and less money that needs to be invested to become a physician, but that is unfortunately the system as it is.
Dr. Leslie Farrington has helped a huge amount of people throughout her career as a practicing healthcare provider and her career as a healthcare advocate. “I just want to inspire people to do something… I want to show research that backs up the claim that racism is why these [health disparities] occur,” she said. Hundreds of thousands of preventable deaths, discomfort within the healthcare system, unaddressed biases… In the United States, healthcare providers as a whole have much room for improvement when dealing with their Black patients. This culture cannot and will not be changed overnight, but with the continued work and dedication from organizations like the Pulse Center for Patient Safety Education & Advocacy and people like Dr. Farrington, the system will be pushed in the right direction.
Pulse Center for Patient Safety, Education and Advocacy: pulsecenterforpatientsafety.org/
By Matt Gonzales
I'd like to thank Dr. Leslie Farrington for sitting for an interview with me.